
NHS needs to understand drug costs better, says ABPI
pharmafile | April 10, 2014 | News story | Medical Communications, Research and Development, Sales and Marketing | ABPI, AGNSS, Deepak Khanna, NICE, Stephen Whitehead, Tarceva, soliris
The UK healthcare system is at risk of failing to adopt new, personalised medicines and must be willing to pay for the cost of innovation.
This is according to an Association of the British Pharmaceutical Industry (ABPI) discussion paper, ‘Securing a Future for Innovative Medicines’, which has been published to coincide with today’s ABPI annual conference in central London.
The report highlights the emergence of specialised medicines as a ‘key challenge’ for the UK pharma industry and says that for the commercial environment in the UK to respond to this challenge, there needs to be a fundamental shift in the Health Technology Assessment (HTA) approach.
The context here is the industry’s long-term frustration with England’s HTA body NICE, which last year did not given a final positive recommendation for any new cancer drug it assessed.
The pricing watchdog argues that these drugs’ costs are too high and with limited relative efficacy to justify their price tags, especially with the NHS budget squeezed and austerity still a major problem in the economy.
Notable examples of personalised medicines being rejected by NICE include Pfizer’s lung cancer drug Xalkori (crizotinib) and Roche’s breast cancer treatment Perjeta (pertuzumab).
NICE has, however, since the beginning of the year recommended a number of new oncology products, including Boehringer’s lung cancer medicine Giotrif (afatinib) and Roche’s lung cancer medicine Tarceva (erlotinib) in a new setting.
But the ABPI notes that changes are occurring in the UK and at a European level, in the form of pioneering joint-working initiatives involving NHS and industry.
Rare diseases, high costs
The report also points to NICE’s Highly Specialised Technology (HST) programme, something which the ABPI believes has the potential to “make a big difference to how specialised medicines for very rare diseases are evaluated”.
But this has also proved a major bone of contention, however, as NICE took over this role from AGNSS last year, but has as yet failed to recommend any orphan drug under its new remit.
In fact the body is currently defending the long delay over Alexion’s Soliris (eculizumab), the first ‘ultra-orphan’ drug to be reviewed by NICE under its new HST process.
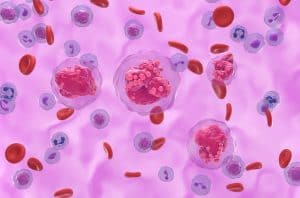
As part of a complex picture, the watchdog has asked the company for more information on the manufacturing, research and development costs of the drug, which is a treatment for the very rare blood disorder known as atypical Haemolytic Uraemic Syndrome (or aHUS).
“Before we can make a confident recommendation for routine use, which we estimate would cost the NHS about £58 million in the first year, rising to over £80 million in five years, we need more information,” NICE’s chief executive Sir Andrew Dillon explained. The drug costs £340,200 ($569,000) per year, per patient.
But the firm has told Pharmafile that it is “concerned that there hasn’t been a decision”, and will have to continue to wait for it to be funded by the NHS.
All of these medicines were costly to create but are equally becoming very costly for healthcare providers to pay for, especially in the state-run NHS.
It is an age-old problem, played out between pharma and HTA bodies for years, but one that seemingly remains unresolved by both parties.
Rising costs, trial problems
The ABPI also highlights further challenges to its members, including rising drug development costs and difficulty with patient recruitment for clinical trials.
The lobby group points out that around 80% of clinical trials do not meet patient recruitment timelines, and on average last 30 – 42% longer than companies initially plan for, therefore increasing costs.
To overcome this, the ABPI wants the UK to improve trial performance by enabling faster patient enrolment, encouraging the use of electronic health records (something the government is now doing) and streamline the research governance process, again something that will be made easier with the EU’s Clinical Trial Regulation last week.
Commenting on the report Stephen Whitehead, chief executive of the ABPI, says: “This report sheds new light on the challenges facing the UK pharmaceutical industry. Whilst companies are refocusing their pipelines towards specialised and stratified medicines, a gap is opening up between the commercial environment the industry currently operates in, and the new research and development (R&D) environment the industry is moving towards.
“If we don’t address this gap soon, patients will be unable to access the best treatments and the UK economy will suffer.
“It is vital that our industry continues to work closely with the NHS and academia to ensure that we become a world leader in stratified medicine, as well as the location of choice for pharmaceutical R&D from across the globe.”
‘The Securing a Future for Innovative Medicines’ discussion paper was prepared for the ABPI by the Office of Health Economics (OHE), which the body funds.
Professor Adrian Towse, director of the OHE, adds: “Global pharmaceutical R&D is changing, and the UK needs to adapt to the new environment in order to retain its status as a leading location for biomedical R&D, both pre and post-launch.
“We must not forget that there are already examples of best practice where changes are occurring in the UK and at European level.
“Only when industry, academia and NHS work together and spread best practice will we better understand how changes in drug development will alter the relationship between the research and commercial elements of the pharmaceutical industry for the NHS.”
Ben Adams
Related Content

NICE recommends migraine treatment for NHS use
The National Institute for Health and Care Excellence (NICE) has shared draft guidance recommending AbbVie’s …

GSK’s Jemperli recommended by NICE for endometrial cancer treatment
GSK has announced that the National Institute for Health and Care Excellence (NICE) has recommended …
NICE recommends SC treatment of AbbVie’s Tepkinly for patients with DLBCL
AbbVie has announced that the National Institute for Health and Care Excellence (NICE) has recommended …








