
NHS to get world’s most expensive drug
pharmafile | November 27, 2014 | News story | Sales and Marketing | Alexion, NICE, aHUS, beauchamp, blood, eculizumab, soliris
UK health watchdog NICE has recommended Alexion’s Soliris for patients with the rare disease atypical haemolytic uremic syndrome (aHUS).
Soliris (eculizumab) is the most expensive drug in the world, and the move sees NHS in England allowing access to the first and only treatment for the condition in a small but growing patient population here – said to number just 200.
Pharmafile spoke to Alexion’s Jon Beauchamp immediately upon hearing the news, who when asked about its huge price tag said: “Final evaluation has now recommended Soliris is funded on the NHS for treatment to aHUS patients, and it has been found to be an appropriate use of NHS funds.
“This has been a long process to arrive here with NICE and we have articulated over the years that its price has to take into consideration the drug’s development costs.”
Soliris is part of the UK’s PPRS scheme, whereby any spend on branded medicines greater than the 2013 spend for the next five years will be refunded by industry.
Beauchamp says this effectively means that any new patient that goes on for treatment in 2014/15 with Soliris, is at no cost to the NHS. For three years beyond that there’s a ‘small amount of allowable growth’ above the 2013 spend – but essentially “it is almost at a zero cost to the NHS for the next five years.”
Leonard Bell, chairman and chief executive of US-based Alexion says: “Today’s decision is an important victory for patients with aHUS. We are pleased that Soliris will be made available on the NHS for patients with aHUS and we commend NHS England for its previous decision to provide interim funding to patients for the extended period it took for NICE to make this final determination.”
Given the increasing focus around NHS spending in the current climate, we asked how the firm reacted to NICE’s previous estimates that Soliris will cost the NHS up to £58 million in the first year – rising to £82 million after five years – with an average patient cost of £330,000 per year.
Beauchamp said: “We submitted our analysis of budget impact and our estimates were significantly lower than those by NICE, which is now acknowledged. NICE said its estimates were in the upper end and we think that’s an exaggeration for some simple reasons – one is it assumes that every single patient that exists with aHUS in the country will be treated from day one, and I’m afraid that will never happen.
“It assumes that every patient is an adult, so the money quoted is an adult cost and a significant portion of these patients are children who receive a lower dose – at a lower cost. Even for the smallest children, the costs are 80% lower than the £327,000 that’s in those estimates.”
But NICE is recommending that the following arrangements need to be in place as conditions for the funding: co-ordination of the use of the drug through an expert center; monitoring systems to record the number of people with diagnosis of aHUS and those who receive Soliris – and their dose and duration of treatment.
It also wants to see a national protocol for starting and stopping Soliris for clinical reasons, and a research programme with robust methods to evaluate when stopping treatment or dose adjustment might occur.
Rare diseases and evaluation
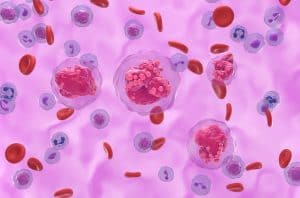
aHUS is a chronic, ultra-rare, and life-threatening disease in which a life-long and permanent genetic deficiency in one or more complement regulatory genes, causes the formation of blood clots in small blood vessels throughout the body.
Asked if the company felt NICE processes were sufficient enough to be dealing with such rare diseases when considering Soliris’s cost-effectiveness, Beauchamp said: “I think its positive that NICE have such a highly specialised process that does appraise rare treatments differently to the more common diseases.
“We were the first to go through it and it was certainly evolving along the way. We were asked for information part way through about the R&D costs specifically, and we didn’t agree with that approach.”
He added that there seems to be a “specific way of looking at medicines in the UK” but that looking more broadly across the globe, Soliris is already approved in many countries in Europe and beyond.
“aHUS is a devastating disease, so also taken into consideration of course is the cost that would be there for not treating it – should Soliris not be available. NICE has said that the magnitude of gain is worth the investment,” Beauchamp concluded.
NICE adds that ‘decisions could change’
Commenting on the draft guidance today, NICE chief executive Sir Andrew Dillon says: “The Committee accepted that eculizumab is a step change in the management of aHUS and can be considered a significant innovation for a disease with a high unmet clinical need.
“Eculizumab offers people with aHUS the possibility of avoiding end-stage renal failure, dialysis and kidney transplantation, as well as other organ damage.
“The drug is, however, very expensive. The Committee felt that the budget impact of eculizumab would be lower if the potential for dose adjustment and stopping treatment was explored.
“This is reflected in the draft guidance which recommends eculizumab should be funded only if important conditions are met, including the development of rules for starting and stopping treatment for clinical reasons. In the meantime NHS England and the company should consider what opportunities might exist to reduce the cost of eculizumab to the NHS.”
Final guidance on the use of Soliris to treat aHUS is expected in January 2015.
Brett Wells
Related Content

NICE recommends migraine treatment for NHS use
The National Institute for Health and Care Excellence (NICE) has shared draft guidance recommending AbbVie’s …

GSK’s Jemperli recommended by NICE for endometrial cancer treatment
GSK has announced that the National Institute for Health and Care Excellence (NICE) has recommended …
NICE recommends SC treatment of AbbVie’s Tepkinly for patients with DLBCL
AbbVie has announced that the National Institute for Health and Care Excellence (NICE) has recommended …








