KCL study could lead to improved vaccinations against STIs
pharmafile | May 23, 2019 | News story | Research and Development | HIV, HSV, STIs, herpes, immune system, std
New findings from researchers at King’s College London could lead to improved vaccinations against sexually transmitted infections (STIs).
Researchers at King’s have shown that a new method involving skin vaccination can generate the protective CD8 T-cells that are recruited to the genital tissues to fight infections as soon as they come into the body – this could help in the development of vaccines for STIs.
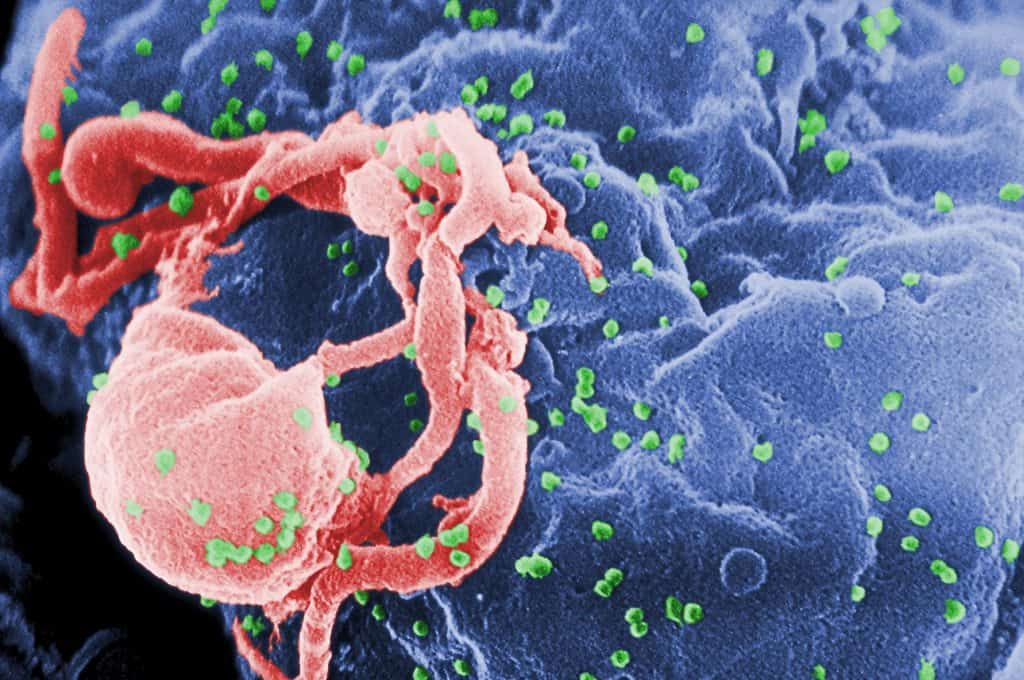
One of the challenges associated with developing vaccines for STIs – including herpes simplex virus (HSV) or HIV – is of attracting CD8 T-cells to the mucosal tissue where the infections first take hold, for example in the female reproductive tract (FRT).
At least two subsets of CD8 T-cells patrol the mucosal tissues as a first line defence. The first lot reside in the tissue ready to defend at a moment’s notice. The second lot circulate between non-lymphoid tissues and the blood.
To protect against STIs, such as HSV and HIV, CD8 T-cells need to be ready to offer immediate protection rather than waiting on immune cells to come from the blood.
In the past, scientists thought that vaccines needed to be delivered directly to the body surface (e.g. female genital tissue), where the infection might start, so that the immune system can generate these CD8 T-cells and send them to the site of infection ready for battle. However, this method of delivering vaccines is neither patient friendly or efficient.
Instead, the team at King’s discovered that their new method of vaccination triggered a process through which immune cells called innate lymphoid cells (ILC1) and monocytes send out signals calling for the mobilisation of CD8 T-cells, which can then protect the host against infection at the front line. Their findings were published in the journal Nature Communications.
Lead author, Professor Linda Klavinskis from King’s said: “This study highlights how specialised groups of ‘innate’ immune cells in distant tissues can be harnessed to attract protective CD8 T-cells, arming the body’s frontline tissues from infection.”
“We now need to confirm these results with other types of vaccines from the one used in the study to see if a common pathway is triggered by skin vaccination. If proven, this could have a significant impact in improving the effectiveness of vaccines against sexually transmitted infections.”
Louis Goss
Related Content

European Commission approves HIV prevention injection
The European Commission (EC) has granted marketing authorisation for Gilead Science’s Yeytuo (lenacapavir), the first …

HIV vaccine candidate successfully optimised for industrial production
Sumagen Canada Inc, a biotech company based in both South Korea and Canada has partnered …

ViiV Healthcare shares data for two-drug regimen for HIV-1 maintenance therapy
GSK has announced that ViiV Healthcare, a specialist HIV company predominantly owned by GSK with …






